M
Mikael Good
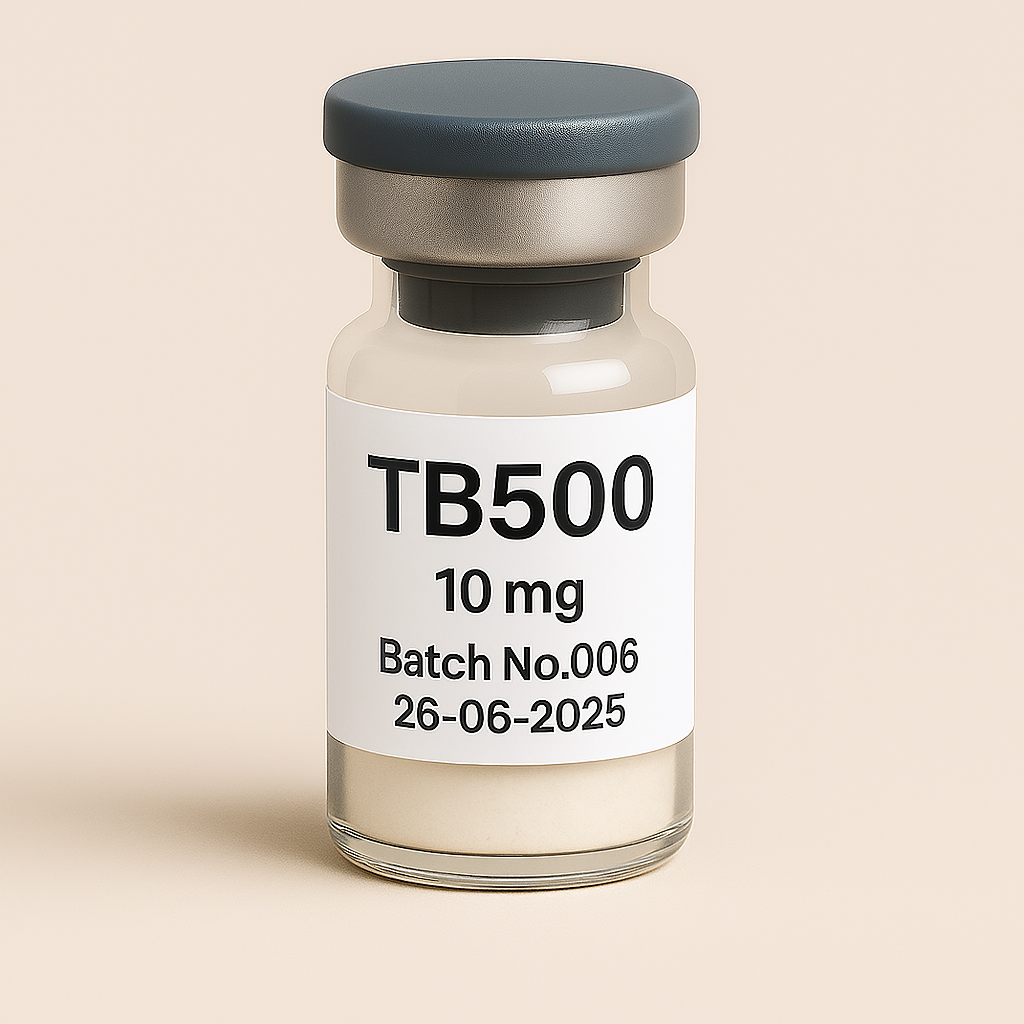
TB500 10mg vial
Pickup currently not available
NOT FOR HUMAN CONSUMPTION
TB-500, also known as Thymosin Beta-4 (Tβ4), is a synthetic peptide derived from a naturally occurring protein found in virtually all human and animal cells. It plays a critical role in cell migration, wound healing, tissue regeneration, and reducing inflammation. Initially discovered in the thymus gland, Thymosin Beta-4 has garnered significant attention in clinical and sports research due to its regenerative and anti-inflammatory properties.
Name: Thymosin Beta-4 (Tβ4), commonly referred to as TB-500 (synthetic form)
Structure: 43-amino-acid peptide
Natural Source: Ubiquitously expressed in various tissues; particularly abundant in wound fluids and platelets
Administration Route: Subcutaneous or intramuscular injection for experimental purposes
Half-life: Approximately 24–48 hours (rapid tissue distribution with prolonged regenerative effects)
TB-500 exerts its effects primarily through:
Promotes cell migration and adhesion, accelerating wound closure and tissue regeneration.
Influences actin polymerization, essential for cell motility and tissue repair.
Stimulates the growth of new blood vessels, improving blood flow, oxygenation, and nutrient delivery to injured tissues.
Reduces inflammatory cytokines and modulates immune responses, facilitating a faster healing process and reduced scar tissue formation.
Exhibits protective effects on cardiac, neural, and muscular tissues, potentially mitigating injury-related damage.
TB-500 demonstrates substantial therapeutic potential across multiple conditions:
Accelerates healing in muscle, tendon, ligament, and joint injuries.
Popular among athletes and bodybuilders experimentally to speed recovery from soft tissue injuries.
Cardioprotective properties following myocardial infarction (heart attack), reducing damage and aiding cardiac repair (animal and preliminary human studies).
Significant improvement in wound closure rates, reduced scar formation, and enhanced skin healing in preclinical models.
Preclinical evidence of neuroprotective benefits in traumatic brain injury (TBI), stroke, and peripheral nerve regeneration.
Experimental potential in treating inflammatory disorders, reducing symptoms, and improving recovery rates.
No standardized clinical guidelines exist, as TB-500 remains experimental. Common dosing strategies used in experimental and anecdotal contexts include:
| Context | Typical Experimental Dose | Administration Frequency |
|---|---|---|
| Soft Tissue Injury and Recovery | 2–4 mg per injection | 1–2 times weekly for 4–6 weeks |
| Maintenance/Chronic Injuries | 2 mg per injection | Once weekly |
| Severe Injuries (Experimental) | Up to 5 mg initially | Twice weekly for initial 2 weeks |
Administration: Usually subcutaneous injection near injury site or general subcutaneous injection.
TB-500 is generally reported as well-tolerated in limited experimental use. However, due to limited clinical studies, complete safety profiles are unknown.
Mild transient irritation or redness at injection sites.
Temporary fatigue or headache (rarely reported).
Limited data on long-term safety in humans.
Theoretical concerns of promoting uncontrolled angiogenesis or tumor growth, though not confirmed in clinical studies.
Contraindications:
Pregnancy and breastfeeding (unknown safety).
Known hypersensitivity or allergic reaction to peptides.
Precautions:
Individuals with active or prior malignancies (theoretical risk of angiogenesis).
Caution in individuals prone to autoimmune conditions or hyperactive immune responses.
Approval Status:
Not approved by FDA or other regulatory agencies for clinical therapeutic use in humans.
Availability:
Typically marketed as a research peptide "not for human consumption."
Sports and Doping:
Explicitly prohibited by World Anti-Doping Agency (WADA) due to regenerative and performance-enhancing potential.
Extensive preclinical (animal) studies confirming regenerative potential for muscle, tendon, ligament injuries, cardiovascular damage, and wound healing.
Limited human clinical studies have been conducted; early trials demonstrate safety and promising efficacy but require further investigation.
Most current human use remains experimental, anecdotal, or investigational, with ongoing research required for robust validation.
| Potential Benefits | Potential Risks and Limitations |
|---|---|
| Accelerated healing of musculoskeletal injuries | Lack of extensive long-term human safety data |
| Anti-inflammatory and reduced scarring effects | Theoretical concerns of angiogenesis and cancer promotion |
| Cardioprotective and neuroprotective properties | Regulatory uncertainty and lack of approved clinical guidelines |
| Potential therapy in chronic inflammatory disorders | Experimental status and limited clinical data |
Conduct large-scale, randomized, controlled human clinical trials to confirm efficacy, dosage optimization, and safety.
Long-term studies assessing safety, potential cancer risk, and impacts on immune function.
Expansion of therapeutic potential investigations into chronic inflammatory, cardiovascular, neurodegenerative, and musculoskeletal conditions.
Sosne, G., & Kleinman, H. K. (2015). "Thymosin Beta 4 promotes dermal healing." Expert Opinion on Biological Therapy, 15(Suppl 1), S47–S53.
Goldstein, A. L., & Hannappel, E. (2005). "Thymosin β4: actin-sequestering protein moonlights to repair injured tissues." Trends in Molecular Medicine, 11(9), 421–429.
Smart, N., Risebro, C. A., & Riley, P. R. (2007). "Thymosin β4 and cardiac repair." Annals of the New York Academy of Sciences, 1112, 82–91.