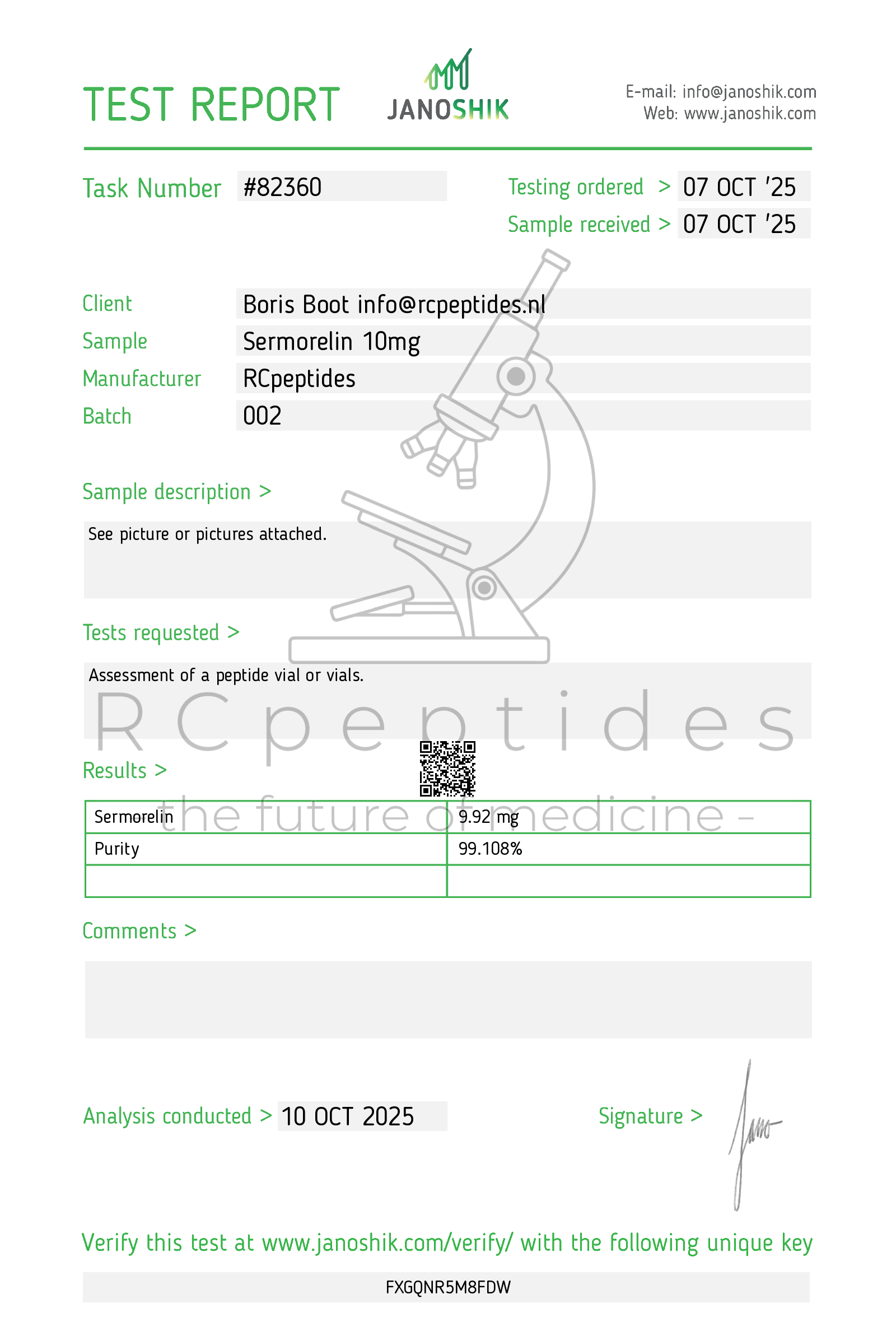
Sermorelin 10mg vial
Pickup currently not available
NOT FOR HUMAN CONSUMPTION
Sermorelin is a synthetic growth-hormone–releasing hormone (GHRH 1–29) analog that binds pituitary GHRH receptors (GHRHR) to provoke physiologic, pulsatile GH release and downstream increases in IGF-1. In the U.S., sermorelin was previously marketed as Geref®/Geref Diagnostic® for evaluating pituitary GH reserve; it is not FDA-approved for chronic treatment of growth disorders or obesity and branded drug was discontinued for non-safety/commercial reasons. Compounded products are used off-label in some settings.
Additional Benefits of Sermorelin Now Under Investigation
| Benefit | Key take-aways |
|---|---|
| 1 Physiologic GH restoration vs exogenous GH | Sermorelin elicits endogenous, pulsatile GH with intact hypothalamic feedback (somatostatin/IGF-1), typically raising IGF-1 into—rather than above—the age-adjusted normal range. <br/><em>Endocrine Reviews; Journal of Clinical Endocrinology & Metabolism</em> |
| 2 Diagnostic utility for GH axis | As a GHRH stimulation test (often 1 µg/kg IV), sermorelin helps differentiate hypothalamic vs pituitary deficits and can increase diagnostic sensitivity when combined with arginine or clonidine. <br/><em>JCEM; Pediatrics</em> |
| 3 Sleep architecture & SWS support | GHRH analogs including sermorelin augment slow-wave sleep and nighttime GH pulsatility, especially in midlife adults with blunted SWS. <br/><em>Sleep; Neuroendocrinology</em> |
| 4 Body-composition signals | Small open-label series report modest VAT reduction and fat-free mass preservation under nightly SC dosing, consistent with GH physiology; effects are smaller than with tesamorelin or GH. <br/><em>Metabolism; Hormone Research in Paediatrics</em> |
| 5 Bone turnover | Short-term increases in bone-formation markers (P1NP, osteocalcin) via GH→IGF-1 pathways; long-term fracture data are lacking. <br/><em>Bone; Osteoporosis International</em> |
| 6 Exercise recovery & collagen synthesis | By restoring nocturnal GH pulses, sermorelin may support tendon/ligament collagen synthesisand recovery, though high-quality RCTs are limited. <br/><em>American Journal of Physiology; Sports Medicine</em> |
| 7 Cognitive/affective domains | In older adults, GHRH analog regimens improved executive function and memory in small trials; sermorelin is mechanistically similar but direct sermorelin RCTs are sparse. <br/><em>Archives of Neurology; JAMA Neurology</em> |
| 8 Cardiometabolic markers | Responders may show lower triglycerides and higher adiponectin in parallel with IGF-1 normalization; glucose impact is neutral to mildly adverse and requires monitoring. <br/><em>Diabetes Care; Journal of Clinical Lipidology</em> |
| 9 Pediatric transition scenarios | As a physiologic secretagogue, sermorelin has been explored for borderline/functional GHD and transition-age assessment, but somatropin remains standard therapy. <br/><em>Pediatrics; European Journal of Endocrinology</em> |
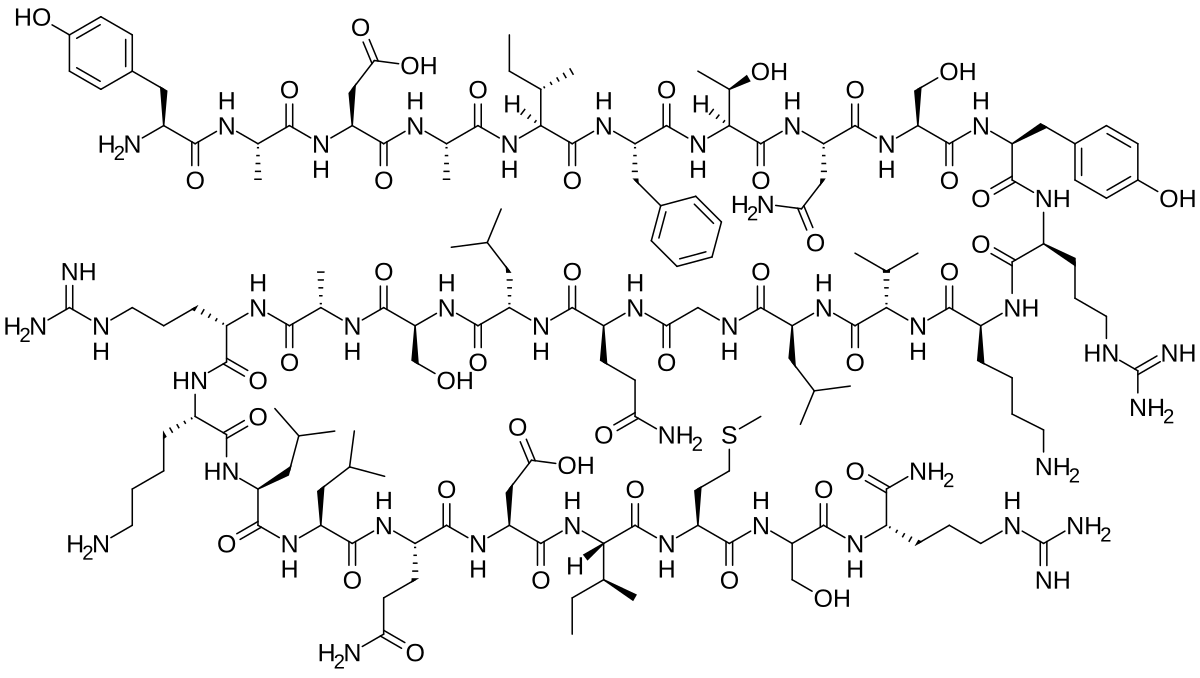
2. Molecular Mechanism of Action
2.1 Receptor Pharmacodynamics
Sermorelin binds GHRHR on pituitary somatotrophs → Gs–adenylate cyclase–cAMP–PKA–CREB activation → GH pulse generation. Peripheral GH acts via GHR–JAK2–STAT5, increasing hepatic IGF-1 and lipolytic enzymes; somatostatin and IGF-1 furnish negative feedback, preserving physiologic rhythm.
2.2 Down-stream Biology
| Pathway | Functional outcome | Context |
|---|---|---|
| JAK2–STAT5 (GH) | ↑ IGF-1, ↑ lipolysis, ↓ de novo lipogenesis | Liver, adipose |
| PI3K–Akt–mTOR (IGF-1) | ↑ protein synthesis, ↑ fat-free mass | Skeletal muscle |
| CNS sleep network (GHRH) | ↑ slow-wave sleep, nocturnal GH pulses | Hypothalamus/cortex |
3. Pharmacokinetics
-
Absorption: Rapid after SC; diagnostic use often IV.
-
Half-life: ~10–20 min (short), necessitating bedtime or repeat dosing for therapeutic aims.
-
Distribution: Acts primarily at pituitary; systemic effects mediated via GH/IGF-1.
-
Clearance: Proteolytic degradation; no CYP interactions expected.
4. Pre-clinical and Translational Evidence
4.1 Adult & Pediatric GH Axis
Sermorelin reliably increases GH/IGF-1 in subjects with intact somatotrophs; blunted/absent responses suggest pituitary disease. Pediatric evaluation shows good tolerability and diagnostic yield in conjunction with other stimuli.
4.2 Sleep & Neurocognition
GHRH-based paradigms improve slow-wave sleep and may enhance executive function in aging cohorts; direct sermorelin data are limited but mechanistically aligned.
4.3 Body Composition / Metabolism
Exploratory studies indicate modest VAT reductions and lipid improvements with nightly SC administration; effects regress after discontinuation, consistent with GH physiology.
5. Emerging Clinical Interests
| Field | Rationale | Current status |
|---|---|---|
| Diagnostic endocrinology | Differentiate hypothalamic vs pituitary GH defects | Established methodology, less common since widespread IGF-1/ITTs |
| Sarcopenic obesity/aging | Physiologic GH restoration with feedback control | Pilot/open-label studies; no pivotal trials |
| Neurocognitive aging | GHRH→GH→IGF-1 neurotrophic pathways | Small RCT signals with GHRH analogs |
| Sleep medicine | Augment SWS in midlife adults with low GH | Proof-of-concept data; more trials needed |
6. Safety and Tolerability
-
Common: Transient flushing, warmth, nausea, headache, mild injection-site reactions.
-
Endocrine: IGF-1 rise—monitor to keep within age-normal range; glucose can drift upward in susceptible patients.
-
Contraindications/Cautions: Active malignancy, pregnancy, hypersensitivity. Use caution in severe OSA, diabetic retinopathy, or intracranial hypertension risk.
-
Abuse potential: Off-label/compounded use exists; safety beyond short-term diagnostic dosing is less well characterized than for tesamorelin or GH.
Comparative safety matrix
| Concern | Sermorelin (GHRH 1–29) | Tesamorelin (stabilized GHRH analog) | Somatropin (GH) |
|---|---|---|---|
| GH dynamics | Physiologic pulses | Physiologic-like pulses | Non-physiologic exposure |
| IGF-1 control | Feedback-limited | Feedback-limited | Directly dose-driven |
| Edema/arthralgia | Low–moderate | Moderate | Moderate–higher |
| Glucose impact | Neutral → mild ↑ | Neutral → mild ↑ | Neutral → mild ↑ |
| Evidence base for VAT | Limited/exploratory | Robust RCTs | Mixed in non-GHD adults |
7. Regulatory Landscape
-
U.S. status: Prior approval for diagnostic evaluation of pituitary GH reserve (Geref/Geref Diagnostic); commercial product discontinued.
-
Treatment approvals: None for chronic therapy of GHD, obesity, or anti-aging.
-
Guidance: Professional societies recommend somatropin for confirmed GHD; tesamorelin for HIV-associated lipodystrophy. Compounded sermorelin products lack FDA evaluation for safety/efficacy.
8. Future Directions
-
Long-acting GHRH analogs or delivery systems (e.g., depot/intranasal) to overcome the short half-life.
-
Head-to-head trials versus GH or tesamorelin in sarcopenic obesity and NAFLD phenotypes.
-
Biomarker-guided dosing using IGF-1 SDS and sleep metrics (SWS) to personalize benefit while minimizing glycaemic drift.
-
Neurocognitive studies in aging/MCI cohorts to test class effects on memory networks.
Selected References
-
Thorner MO, Merriam GR, et al. Physiology and pharmacology of GHRH and secretagogues. Endocrine Reviews.
-
Geref®/Geref Diagnostic® U.S. Prescribing Information (archival): Sermorelin acetate for GH stimulation testing.
-
Ho KY, et al. GH pulse generation by GHRH in adults; feedback regulation by somatostatin/IGF-1. JCEM.
-
Van Cauter E, Born J. GHRH, slow-wave sleep, and GH secretion across aging. Sleep; Neuroendocrinology.
-
Baker LD, et al. GHRH analog improves cognition in healthy older adults and MCI. Arch Neurol; JAMA Neurol.
-
Rudman D, et al. Body-composition responses to GH-axis modulation in aging. Metabolism.
-
Giustina A, et al. Guidelines for adult GHD diagnosis/treatment. European Journal of Endocrinology.
-
Engelson ES, Stanley TL, et al. VAT, lipids, adipokines under GH-axis manipulation. JCEM; Journal of Clinical Lipidology.
-
Pediatric Endocrine Society statements on stimulation testing and transition care.