Methylene blue USP grade 100x10mg
Pickup currently not available
NOT FOR HUMAN CONSUMPTION
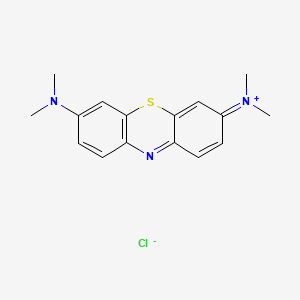
Methylene blue is a phenothiazine redox dye with multiple pharmacologies. Clinically it’s FDA-approved for acquired methemoglobinemia (it accepts electrons from NADPH-methemoglobin reductase as leucomethylene blueand reduces Fe³⁺→Fe²⁺ to restore O₂ carriage). Beyond this, MB inhibits nitric-oxide synthase and soluble guanylyl cyclase (sGC) (countering pathologic vasodilation), acts as a photosensitizer for antimicrobial photodynamic therapy (aPDT), shuttles electrons in mitochondria, and is a potent reversible MAO-A inhibitor (important for drug interactions).
Additional Benefits of Methylene Blue Now Under Investigation
| Benefit | Key take-aways |
|---|---|
| 1 Vasoplegic shock rescue (sepsis/post-CPB) | IV MB can raise MAP and reduce catecholamine dose by blocking NO–sGC–cGMP signalling; early use in vasoplegia (post-cardiac surgery, septic shock) shows hemodynamic benefit in RCTs/series; mortality data remain mixed. <br/><em>Critical Care; Anesthesiology</em> |
| 2 Ifosfamide-induced encephalopathy | Case series and protocols support 1–2 mg/kg IV q4–8 h to reverse neurotoxicity, likely via redox re-routing (NAD⁺/NADH) and monoamine oxidase modulation. <br/><em>Journal of Clinical Oncology; Supportive Care in Cancer</em> |
| 3 Tau aggregation & neurodegeneration | MB/LMTM (leuco-methylthioninium) inhibits tau aggregation and supports mitochondria; Alzheimer’s trials show mixed outcomes (signals in monotherapy subsets), with dosing/formulation under refinement. <br/><em>Journal of Alzheimer’s Disease; The Lancet Neurology</em> |
| 4 Mitochondrial rescue & neuroprotection | At low doses, MB bypasses complex I/III blocks, improves ATP generation, reduces ROS, and shows retinal/optic-nerve protection in models and small studies. <br/><em>PNAS; Investigative Ophthalmology & Visual Science</em> |
| 5 Antimicrobial photodynamic therapy (aPDT) | MB + 630–670 nm light produces singlet oxygen, killing planktonic and biofilm bacteria (including MRSA/P. aeruginosa) and fungi; used in chronic wounds, dentistry, ENT pilots. <br/><em>Antimicrobial Agents & Chemotherapy; Journal of Clinical Periodontology</em> |
| 6 Antimalarial partner & transmission-blocking | Added to artemisinin regimens, MB lowers gametocytemia and may reduce transmission; GI/urine discoloration and G6PD-related hemolysis risk require screening. <br/><em>The Lancet Infectious Diseases; Malaria Journal</em> |
| 7 Dermatologic/anti-photoaging (topical) | MB creams show fibroblast rejuvenation, ↑ collagen genes, ↓ senescence markers, and improved hydration/wrinkles in small trials. <br/><em>Redox Biology; Dermatologic Therapy</em> |
| 8 Refractory ischemic priapism | Intracavernosal MB inhibits NO–sGC, offering rescue when alpha-agonists fail before shunting. <br/><em>Urology; BJU International</em> |
| 9 Peri-anaphylaxis vasoplegia | As adjunct in refractory hypotension after anaphylaxis or spinal anesthesia, MB can restore vascular tone via sGC blockade; evidence largely from series. <br/><em>Annals of Allergy, Asthma & Immunology; British Journal of Anaesthesia</em> |
2. Molecular Mechanism of Action
2.1 Target Pharmacodynamics
-
RBC redox cycling: MB ⇄ leucomethylene blue accepts electrons from NADPH-MetHb reductase, reducing MetHb → Hb.
-
Vascular tone: NOS and sGC inhibition ↓ cGMP → reverses pathologic vasodilation in vasoplegia.
-
MAO-A inhibition: Potent, reversible inhibition → serotonin-syndrome risk with serotonergic drugs.
-
Mitochondrial electron shuttle: Accepts/donates electrons between NADH ↔ cytochrome c, bypassing ETC blocks.
-
Photosensitizer: Upon red-light activation, generates singlet oxygen/ROS for aPDT.
2.2 Down-stream Biology
| Pathway | Functional outcome | Context |
|---|---|---|
| NADPH-MetHb reductase | Restores O₂ carriage | Methemoglobinemia |
| NO–sGC–cGMP axis | ↑ MAP, vasoconstrictive tone | Vasoplegic shock, priapism |
| MAO-A inhibition | ↑ synaptic monoamines; DDI risk | CNS/pharmacology |
| ETC bypass (redox) | ↑ ATP, ↓ ROS | Neuro/retina, ischemia–reperfusion |
| aPDT (ROS burst) | Rapid microbicidal & anti-biofilm | Wounds, dental/ENT |
3. Pharmacokinetics
-
Routes: IV (methemoglobinemia, vasoplegia), oral (historical/adjunct), topical, intracavernosal (rescue), intranasal/neb (investigational aPDT).
-
Onset: IV minutes for MetHb/MAP effects.
-
Half-life: Biphasic; reports ~5–24 h (formulation-dependent).
-
Distribution/biotransformation: Rapid tissue distribution; reduced to leuco-MB intracellularly; renal excretion(blue-green urine), some biliary.
-
Device interference: Transient SpO₂ under-reading (absorbs at 660 nm).
4. Pre-clinical and Translational Evidence
4.1 Vasoplegic Syndromes
In sepsis and post-cardiopulmonary-bypass vasoplegia, MB improves MAP and reduces vasopressor needs; timing (early vs rescue), dose, and patient selection are key determinants; outcome effects are under active study.
4.2 Oncology/Neurodegeneration
Tau-targeting LMTM programs show dose/formulation-dependent cognitive outcomes; mitochondrial support and anti-aggregation continue to be explored in AD/FTD.
4.3 Anti-infective aPDT
Topical/oral cavity MB-aPDT clears biofilms, reduces peri-implant mucositis/periodontitis indices, and accelerates chronic-wound granulation; standardized dosing and light fluence remain to be harmonized.
4.4 Ifosfamide Encephalopathy & Others
Observational cohorts report neurologic recovery after MB in IIE; additional uses include priapism rescue, sentinel-node mapping, and urologic staining.
Evidence quality note: Robust for methemoglobinemia; moderate/heterogeneous for vasoplegia and IIE (controlled but small); emerging for aPDT, dermatology, and neurodegeneration.
5. Emerging Clinical Interests
| Field | Rationale | Current status |
|---|---|---|
| Vasoplegic shock (sepsis/post-CPB) | sGC blockade complements vasopressors | RCTs/series; practice heterogeneity |
| Ifosfamide encephalopathy | Redox/MAO pathways | Protocolized rescue in centers |
| Alzheimer’s/FTD (LMTM) | Tau inhibition + mitochondrial support | Mixed trials; next-gen formulations |
| Chronic wounds/dentistry (aPDT) | Anti-biofilm + pro-healing | Early clinical adoption |
| Retinal/optic neuroprotection | ETC bypass, anti-ROS | Small human/mechanistic |
| Antimalarial partner | Gametocyte kill/transmission block | Regional trials |
| Priapism (refractory) | NO–sGC inhibition | Salvage case series |
6. Safety and Tolerability
-
Common: Blue/green urine, skin/scleral tint, nausea, dizziness, headache, dysgeusia.
-
Hematology: Hemolysis risk in G6PD deficiency; screen when feasible. High doses can worsen methemoglobinemia (paradoxical).
-
Neurologic/psychiatric: Serotonin syndrome possible with SSRIs/SNRIs/MAOIs/linezolid/tramadol, etc. (MB is a potent MAO-A inhibitor).
-
Cardiovascular: ↑ SVR/MAP desired in vasoplegia; watch for hypertension/ischemia in susceptible patients.
-
Pulmonary: Can transiently lower SpO₂ readings (optical artifact).
-
Pregnancy/Neonates: Avoid—risk of fetal/neonatal hemolysis and hyperbilirubinemia; crosses placenta.
-
Dosing considerations: Typical IV 1–2 mg/kg (slow push/infusion) with repeat dosing per protocol; monitor MetHb, ABG, hemodynamics.
Comparative safety matrix (vasoplegia context)
| Concern | Methylene blue | Hydroxocobalamin | Vasopressin |
|---|---|---|---|
| Primary mechanism | NOS/sGC inhibition | NO scavenger (cobalt) | V1 receptor agonist |
| Effect on MAP | Rapid ↑; catecholamine-sparing | Rapid ↑; catecholamine-sparing | ↑ SVR with low arrhythmia risk |
| Key risks | MAO-A DDIs, G6PD hemolysis, SpO₂ artifact | Chromaturia, potential oxalate, interference with labs | Ischemia at high dose, hyponatremia |
| Special notes | Can worsen MetHb at high dose | Useful when MB contraindicated | Synergizes with MB in rescue |
7. Regulatory Landscape
-
Approved: Acquired methemoglobinemia (parenteral MB).
-
Common off-label: Vasoplegic shock, ifosfamide encephalopathy, priapism rescue, aPDT (topical/oral cavity).
-
Investigational: Tau-targeting LMTM, retinal neuroprotection, antimalarial partner.
-
Supply: Use GMP-grade MB (sterile, USP) for IV; compounded/non-sterile dyes are unsafe IV.
8. Future Directions
-
Precision use in vasoplegia: Timing (early vs rescue), dose–response, and phenotype selection (e.g., high NO/cGMP signatures).
-
Neurodegeneration: Optimize LMTM pharmacokinetics and identify tau-positive, monotherapy-responsivesubgroups.
-
Standardize aPDT: Dose, fluence, and outcomes for wounds/dentistry/ENT; head-to-head vs antibiotics.
-
Mitochondrial medicine: Define dose window for ETC support without MAO-A adverse effects.
-
Safety registries: Serotonin-syndrome pharmacovigilance; G6PD screening pathways; pregnancy/neonatal outcomes.
Selected References
-
Anesthesiology; Critical Care — Vasoplegic shock trials/series with MB (post-CPB, sepsis).
-
Journal of Clinical Oncology; Supportive Care in Cancer — Ifosfamide-induced encephalopathy reversal protocols.
-
The Lancet Neurology; Journal of Alzheimer’s Disease — LMTM (methylthioninium) in tauopathies.
-
PNAS; Redox Biology — Mitochondrial electron-shuttling and antioxidant properties.
-
Antimicrobial Agents & Chemotherapy; Journal of Clinical Periodontology — MB-mediated aPDT in wounds/dentistry.
-
The Lancet Infectious Diseases; Malaria Journal — MB as an antimalarial partner and transmission-blocking agent.
-
Investigative Ophthalmology & Visual Science — Retinal/optic neuroprotection studies.
-
Urology; BJU International — MB for refractory priapism via NO–sGC inhibition.