Triptorelin Acetate 10mg vial
Abholung derzeit nicht verfügbar
NOT FOR HUMAN CONSUMPTION
Triptorelin is a long-acting gonadotropin-releasing hormone (GnRH/LHRH) agonist. After an initial LH/FSH “flare”, continued receptor stimulation on pituitary gonadotrophs causes desensitization/internalization and suppression of gonadotropins, leading to medical castration (↓ testosterone/estradiol). It is widely approved for advanced prostate cancer, central precocious puberty (CPP), and (ex-US) endometriosis, uterine fibroids, and assisted reproductiondown-regulation. Depot IM/SC formulations (e.g., 1-, 3-, 6-month) provide sustained exposure.
Additional Benefits of Triptorelin Now Under Investigation
| Benefit | Key take-aways |
|---|---|
| 1 Optimized prostate-cancer control in combinations | As the ADT backbone, triptorelin pairs with androgen-receptor pathway inhibitors(abiraterone, apalutamide, enzalutamide, darolutamide) in mHSPC/mCRPC to improve survival versus ADT alone. <br/><em>European Urology; Lancet Oncology</em> |
| 2 Intermittent ADT strategies | Intermittent triptorelin-based ADT can maintain disease control with better quality of life in selected patients; ongoing work refines PSA-based cycling criteria. <br/><em>NEJM; Journal of Clinical Oncology</em> |
| 3 Cardiometabolic risk management | Programs evaluate baselining CV risk, exercise/nutrition, and statin/SGLT2/GLP-1RA co-therapy to mitigate ADT-related dysmetabolism while on triptorelin. <br/><em>Circulation; JACC: CardioOncology</em> |
| 4 Ovarian function suppression (OFS) in HR+ breast cancer | In premenopausal ER+ disease, triptorelin-based OFS plus tamoxifen or aromatase inhibitor improves disease-free survival versus endocrine therapy alone. <br/><em>NEJM; Journal of Clinical Oncology</em> |
| 5 Fertility preservation during chemotherapy | Temporary ovarian suppression with triptorelin during cytotoxic therapy reduces premature ovarian insufficiency and may increase post-treatment pregnancy rates. <br/><em>JAMA; Annals of Oncology</em> |
| 6 Endometriosis & adenomyosis control | 3–6 months of depot therapy reduces pelvic pain and lesion activity; add-back therapy helps bone and vasomotor tolerability during prolonged courses. <br/><em>Human Reproduction Update; BJOG</em> |
| 7 Uterine fibroids (pre-op or bridging) | Pre-operative triptorelin shrinks fibroids and improves anaemia, easing surgical approaches or bridging to definitive therapy. <br/><em>Fertility and Sterility; Obstetrics & Gynecology</em> |
| 8 IVF/ART down-regulation | Long-protocol down-regulation with triptorelin prevents premature LH surge and can standardize follicular recruitment; antagonist protocols now compete—comparative trials continue. <br/><em>Reproductive BioMedicine Online; Human Reproduction</em> |
| 9 CPP convenience & adherence | 6-month depot schedules sustain T/E2 suppression with fewer injections and robust bone-age/height-velocity control. <br/><em>Pediatrics; Journal of Clinical Endocrinology & Metabolism</em> |
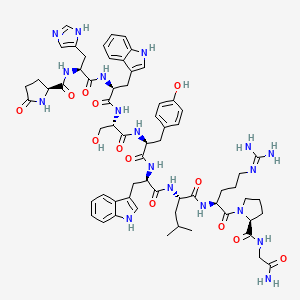
2. Molecular Mechanism of Action
2.1 Receptor Pharmacodynamics
Triptorelin binds GnRH (GNRHR) GPCR on pituitary gonadotrophs → Gαq/11–PLCβ–IP₃/DAG–Ca²⁺/PKC → acute LH/FSH release (“flare,” days 1–7). Continuous exposure triggers receptor desensitization/internalization, suppressing LH/FSH and downstream testicular/ovarian steroidogenesis.
2.2 Down-stream Biology
| Pathway | Functional outcome | Context |
|---|---|---|
| IP₃/Ca²⁺/PKC→ERK | Acute LH/FSH secretion | Pituitary |
| ↓ GnRH signalling (chronic) | ↓ LHB/FSHB transcription, gonadotropin suppression | Pituitary |
| ↓ LH→Leydig / ↓ FSH→Sertoli | ↓ Testosterone; impaired spermatogenesis | Testis |
| ↓ LH/FSH→Ovary | ↓ Estradiol/progesterone; anovulation | Ovary |
3. Pharmacokinetics
-
Formulations: Microsphere depots (e.g., 3.75 mg q4wk; 11.25 mg q12wk; 22.5 mg q24wk) and pediatric 24-week depot for CPP.
-
Absorption: Initial burst → sustained zero-order-like release from PLGA matrix.
-
Onset: Steroid “flare” within first week; castrate T typically by 2–4 weeks.
-
Half-life: Parent peptide t½ is short (hours) but effective duration reflects depot kinetics (1–6 months).
-
Clearance: Peptidase degradation; renal/hepatic peptide catabolism; no CYP interactions.
4. Pre-clinical and Translational Evidence
4.1 Prostate Cancer (ADT backbone)
Triptorelin achieves durable castration with PSA responses comparable to other agonists; combinations with AR pathway inhibitors significantly prolong rPFS/OS versus ADT alone.
4.2 Breast Cancer (premenopausal, HR+)
In SOFT/TEXT-style regimens, OFS with triptorelin plus tamoxifen or an aromatase inhibitor improves invasive disease-free survival, particularly in higher-risk patients.
4.3 CPP
Depot triptorelin suppresses pubertal progression, normalizes growth velocity, and improves predicted adult height, with convenient 6-month dosing options.
4.4 Endometriosis/Fibroids/ART
In endometriosis and fibroid protocols, triptorelin reduces estrogen-driven activity, facilitating symptom control and surgery. In IVF, long down-regulation prevents premature LH surge; antagonist regimens provide alternative flexibility.
5. Emerging Clinical Interests
| Field | Rationale | Current status |
|---|---|---|
| ADT + cardiometabolic co-management | Reduce CV events during long-term ADT | Prospective cardio-oncology programs |
| Intermittent ADT | QoL vs continuous ADT in mHSPC/biochemical relapse | Ongoing refinement, patient-selected |
| OFS personalization | Tailor duration/intensity in HR+ breast cancer | Risk-adapted strategies under study |
| Non-binary/trans care | GnRH analogs for puberty suppression/adult OFS | Practice varies by region; triptorelin used ex-US |
6. Safety and Tolerability
-
Common: Hot flashes, decreased libido, erectile/sexual dysfunction, mood change, headache, injection-site reactions.
-
Metabolic/Bone: Weight gain, insulin resistance, dyslipidemia, bone-mineral density loss (consider DXA and bisphosphonate/denosumab in long-term ADT/OFS).
-
On-treatment flare (men): Transient tumor-flare may cause bone pain, urinary obstruction, spinal cord compression—use antiandrogen lead-in/overlap in metastatic settings.
-
Women: Vasomotor symptoms, amenorrhea, initial ovarian cysts possible; use add-back therapy for longer courses.
-
Pediatrics: Initial pubertal signs may transiently appear; monitor height velocity and bone age.
-
Rare: Pituitary apoplexy shortly after first dose in patients with undiagnosed adenomas; immediate evaluation if severe headache/visual change.
Comparative safety matrix
| Concern | Triptorelin (GnRH agonist) | GnRH antagonists (degarelix, relugolix) | Orchiectomy / Oophorectomy |
|---|---|---|---|
| On-treatment flare | Yes (mitigate with antiandrogen) | No | No |
| Time to castration | 2–4 weeks | 1–2 weeks (faster) | Immediate |
| CV risk signal | Class concern | Some studies suggest lower CV events | Baseline surgical risks |
| Convenience | Monthly–6-monthly depot | Monthly depot or daily oral | One-time procedure |
| Reversibility | Yes (after depot wanes) | Yes | No |
7. Regulatory Landscape
-
Approved: Prostate cancer (ADT) and CPP (varies by region/formulation).
-
Common ex-US uses: Endometriosis, uterine fibroids, ART down-regulation.
-
Monitoring: For ADT/OFS, monitor T/E2 levels, metabolic panel, BMD, and disease markers (e.g., PSA).
-
Contraindications: Pregnancy, breastfeeding, hypersensitivity to GnRH analogs; caution in severe osteoporosisand unstable metastases (flare risk).
8. Future Directions
-
Depot innovation: Longer-acting and smaller-volume depots; SC auto-injectors.
-
Precision ADT/OFS: Risk-adapted durations, biomarker-guided restart/stop rules (PSA kinetics, ultrasensitive E2).
-
Cardio-oncology pathways: Integrated CV risk mitigation embedded in ADT protocols.
-
Combination trials: Triplet regimens (ADT + ARSI + RT/chemo) and de-escalation after deep responses.
-
Pediatric CPP: Long-term neurocognitive and bone outcomes with extended 6-month dosing.
Selected References
-
European Urology; Lancet Oncology — ADT backbones and AR-targeted combinations in mHSPC/mCRPC.
-
New England Journal of Medicine; Journal of Clinical Oncology — Intermittent vs continuous ADT; OFS in premenopausal HR+ breast cancer.
-
JAMA; Annals of Oncology — Ovarian suppression during chemotherapy and fertility preservation.
-
Human Reproduction Update; BJOG — Endometriosis/adenomyosis management with GnRH agonists and add-back therapy.
-
Fertility and Sterility; Obstetrics & Gynecology — Uterine fibroid pre-operative shrinkage and ART down-regulation protocols.
-
Pediatrics; JCEM — CPP efficacy, growth and bone-age outcomes with long-interval depots.
-
Circulation; JACC: CardioOncology — Cardiometabolic risk and mitigation during ADT